◉背景
对于直径≤2cm的浸润性外周非小细胞肺癌,肺段切除术与肺叶切除术的比较。
◉方法
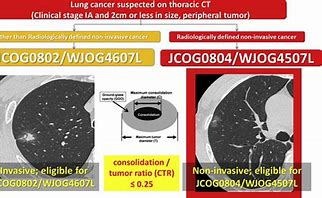
● 研究设计:Ⅲ期临床研究
● 研究对象:直径≤2cm的浸润性外周非小细胞肺癌,计划入组1100 例患者
- 年龄20至85岁
- 单个肿瘤,疑似NSCLC,肿瘤中心位于肺野外三分之一,肿瘤不位于中叶,无淋巴结转移。
- 最大肿瘤直径≤2 cm和肿瘤C/T比> 0.5。该方案在入组4年后进行了修订,根据先前JCOG研究(JCOG0201)的结果,将入组标准从C / T比率> 0.25改为> 0.5,其中肿瘤≤3cm,C / T比值≤0.5的患者显示无复发生存期足够好(5年无复发生存率,95.9%)。
- 预计术后1.0秒用力呼气量(FEV1)≥800毫升,动脉氧张力≥65 Torr。
● 干预措施:随机接受肺叶切除术或肺段切除术。
- 肺段切除术分为简单和复杂。简单的肺段切除术定义为右侧或左侧第6段、左上叶固有段或舌段的肺段段切除。这些段的切除很简单,因为只有1个段间平面可以识别。
- 复杂的肺段切除术是切除简单肺段之外的其他肺段,或者切除任何具有超过1个段间平面的肺段。
- 肺叶切除术包括切除除中叶以外的肺叶。不允许切除超过1个肺叶。
- 肺段切除术定义为切除一个肺段或一个肺段及另外的相邻段;但基底段切除术不被视为肺段切除术。
- 手术切缘,切口末端未被内脏胸膜覆盖的距离与肿瘤边缘进行宏观评估,以确认手术切缘不小于最大肿瘤直径或20 mm。否则,在关闭胸壁之前,必须进行冰冻切片或细胞学病理检查以确认切口末端的无肿瘤状态。当边缘为阳性时,必须进行另外的切除。
- 当纯GGO位于不同的肺叶时,首先推荐随访而不是切除,然而,切除也是可接受的选择。
- 建议对纵隔淋巴结进行系统清扫,但也接受了选择性清扫。选择性淋巴结清扫术是对位于上叶的肿瘤的进行上纵隔淋巴结清扫,对位于下叶的肿瘤进行下纵隔淋巴结清扫。通过冷冻切片诊断检查可见的肿大淋巴结,如果发现肿瘤细胞阳性,则完全切除需要手术模式的改变。淋巴结采样是不可接受的。
● 研究终点:
- 主要终点是所有随机化患者的OS。
- 次要终点为术后呼吸功能,无复发生存率,局部复发比例,不良事件,肺段切除完成比例,住院时间,胸管置入持续时间,手术时间,术中出血量,使用的自动缝合器。不良事件,肺段切除术完成的比例,失血量,胸管放置持续时间以及使用的自动缝合器的数量。
- 术后早期并发症定义为手术后30天内发生的并发症。使用不良事件的通用术语标准3.0版评估并发症。关于术后瘘/肺-肺腔(即漏气),在胸腔引流期间使用以下标准:0级=无;1级=轻度,无需其他治疗;2级=术后延长置管超过7天或需要胸膜粘连治疗;3级=需要再次手术;4级=危及生命。肺并发症定义为瘘/肺-胸腔(即漏气)和/或胸膜感染(即脓胸)。
◉ 结果
● 生存:
- 肺段切除术组的5年和10年OS分别为94.3%(95%CI:92.1–96.0%)和83.6%(95% CI:80.0–86.5%),而肺叶切除术组分别为91.1%(95% CI:88.4–93.2%)和79.8%(95% CI:76.1–83.0%)。术后5年和10年时,肺段切除术与肺叶切除术在OS上的差异分别为3.2%和3.8%,支持肺段切除术(风险比[HR] 0.864;95% CI 0.668-1.119)。
- 肺段切除术组的5年RFS为88.0%(95% CI:85.0–90.4%),肺叶切除术组为87.9%(95% CI:84.8–90.3%);10年RFS分别为76.8%(95% CI:72.9–80.2%)和78.0%(95% CI:74.2–81.3%)(HR 1.050;95% CI 0.828-1.333)。肺段组 12.8% vs 肺叶组 8.4%。局部+区域复发:肺段组 11.2% vs 肺叶组 5.8%。
● 安全性:
- 没有死亡。肺叶切除术和肺段切除术组的并发症(≥2级)分别为26.2%和27.4%(P = .68)。肺叶切除术和肺段切除术组分别检出21例(3.8%)和36例(6.5%)患者的瘘/肺-胸腔(漏气)( P = .04)。多变量分析显示肺部并发症的预测因素,包括漏气和脓胸(≥2级),复杂的肺段切除术(与肺叶切除术相比)(优势比,2.07; 95%置信区间,1.11-3.88; P = .023),和> 20每年吸烟年数(优势比,2.61; 95%置信区间,1.14-5.97; P = .023)。除了在肺段切除术组中观察到更多的漏气 之外,肺叶切除术和肺段切除术患者的术中和术后并发症的几乎没有差异。
- 肺功能:术前预期:肺段组比肺叶组至少好10%。实际结果:术后6个月好2.7%,1年好3.5%,“未达到预设的临床意义阈值”。
◉ 结论
- 肺段切除术相对肺叶切除术无总生存优势,但不劣于肺叶切除术;
- 肺段切除术较肺叶切除术有更多的局部复发率;
- 肺段切除术较肺叶切除术未保留更多肺功能。
- 肺叶切除术仍然是周围型浸润性肺癌的标准术式。
◉ 评论
与肺叶切除相比,肺段切除术并不总是创伤性较小,复杂的肺段切除术可能导致术后早期肺部疾病的发生。
◉ 存在问题
◉ 相似研究
○ ● ◎
相关文献:
评论
相似研究
JCOG 0802系列文献- Saji H, Okada M, Tsuboi M, Nakajima R, Suzuki K, Aokage K, Aoki T, Okami J, Yoshino I, Ito H, Okumura N, Yamaguchi M, Ikeda N, Wakabayashi M, Nakamura K, Fukuda H, Nakamura S, Mitsudomi T, Watanabe SI, Asamura H; West Japan Oncology Group and Japan Clinical Oncology Group. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. 2022 Apr 23;399(10335):1607-1617. doi: 10.1016/S0140-6736(21)02333-3. PMID: 35461558. 5年OS,肺段优于肺叶
- Suzuki K , et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg. 2019 手术并发症相似
- Hattori A , et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer with radiologically pure-solid appearance in Japan (JCOG0802/WJOG4607L): a post-hoc supplemental analysis of a multicentre, open-label, phase 3 trial. Lancet Respir Med. 2024. 纯实性结节,RFS 肺叶优于肺段切除术,尤其是在<70岁,女性人群
- Maniwa T, et al. Lymph node dissection in small peripheral lung cancer: Supplemental analysis of JCOG0802/WJOG4607L. J Thorac Cardiovasc Surg. 2024. 淋巴结清扫:部分实性结节邻近叶间和纵隔淋巴结清扫不影响分期,实性结节至少应行选择性清扫
- Nakagawa K , et al. Risk Factors for Locoregional Relapse After Segmentectomy: Supplementary Analysis of the JCOG0802/WJOG4607L Trial. J Thorac Oncol. 2025. 纯实性结节、切缘距离小于肿瘤大小和男性与肺段切除术局部复发率高显著相关。
- Ryu Nakajima, et al. Long-Term Outcomes of Segmentectomy Versus Lobectomy in Small-Sized Peripheral Non-Small Cell Lung Cancer: A 10-Year Follow-Up Analysis of the Phase 3 Randomized Trial (JCOG0802/WJOG4607L). AATS, 2025. 10年OS,两组相似
- Akamine K, et al. Segmentectomy versus lobectomy in small-sized, peripheral, and pathologically invasive non-small cell lung cancer: Supplemental analysis of JCOG0802/WJOG4607L. AATS, 2025. 病理上有浸润性癌特征,肺段切除术局部复发率高,但生存至少不劣于肺叶切除术
|
|